When experiencing a twisted joint in the lower leg, immediate action is essential to reduce swelling and prevent further damage. Begin by applying a cold compress to the affected area for 15-20 minutes every 2-3 hours during the first 48 hours. This helps minimize inflammation and limits discomfort. Elevate the limb to heart level whenever possible to encourage fluid drainage and prevent pooling of blood in the area.
Rest is critical for recovery. Avoid putting weight on the injured joint and use crutches or a support brace if necessary. This reduces strain on the ligaments and allows for healing. Overexerting the foot by walking or running too soon can lead to prolonged recovery and increased risk of reinjury.
Once the initial swelling has subsided, gentle exercises may be introduced to restore mobility and strength. Focus on exercises that involve controlled movement, ensuring that the joint does not move beyond a safe range of motion. A gradual increase in intensity helps rebuild muscle strength around the joint, which is essential for stability and future prevention.
For severe cases where mobility remains impaired despite conservative treatment, consulting a medical professional for further assessment is advised. An X-ray or MRI might be necessary to rule out fractures or other serious issues that could delay the recovery process.
Understanding the Injury and Treatment Process
For immediate relief, follow the R.I.C.E. method: Rest, Ice, Compression, and Elevation. Apply ice within the first 48 hours to reduce swelling, but limit each session to 20 minutes to prevent frostbite. Keep the affected limb elevated above heart level to help minimize swelling.
Avoid walking or putting weight on the injured area during the first few days to prevent further damage. Use crutches or a brace to support the injury and provide stability while moving. As swelling reduces, begin gentle range-of-motion exercises to avoid stiffness.
Consult a medical professional if pain persists or if mobility is limited, as this could indicate a more severe injury requiring further intervention, such as physical therapy or imaging tests like X-rays to rule out fractures.
Understanding the Types of Ankle Injuries
When an individual sustains an injury to the lower leg joint, it is essential to identify the type of damage in order to apply the correct treatment. Injuries can be categorized based on the ligaments affected and the severity of the trauma.
Type I: Mild Damage – This type involves slight overstretching or microscopic tears in the ligaments. Symptoms typically include mild swelling and discomfort, often without significant bruising. Rest, ice, compression, and elevation (R.I.C.E.) are recommended for recovery.
Type II: Moderate Injury – In this case, there are partial tears of the ligaments, leading to more noticeable swelling, bruising, and instability in the joint. This injury often requires a more extended period of rest, support (such as bracing), and physical therapy to restore strength and flexibility.
Type III: Severe Tear – This type involves a complete rupture of the ligaments, resulting in significant joint instability, swelling, and bruising. Immediate medical attention is necessary, and in some cases, surgical intervention may be required to repair the damaged tissues.
Proper rehabilitation for all types of injury is crucial for long-term mobility and function. Each type demands a tailored approach to ensure the injured area heals correctly and does not lead to recurring issues.
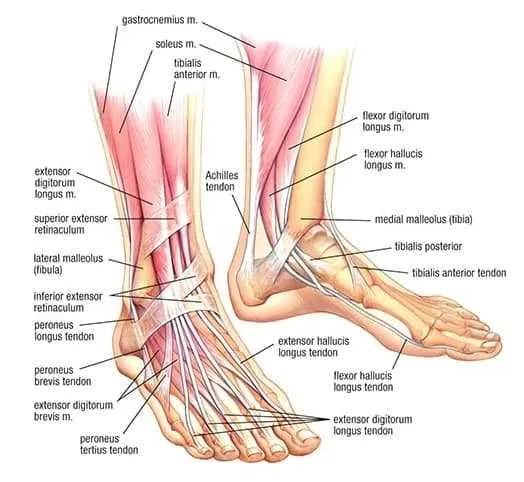
Key Muscles and Ligaments Affected in an Injured Foot Joint
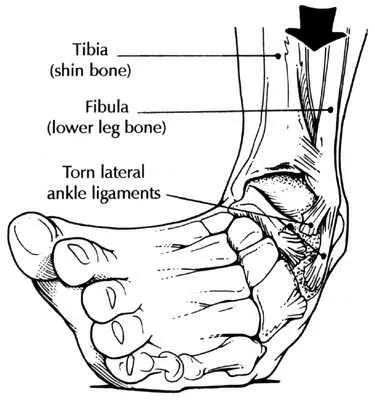
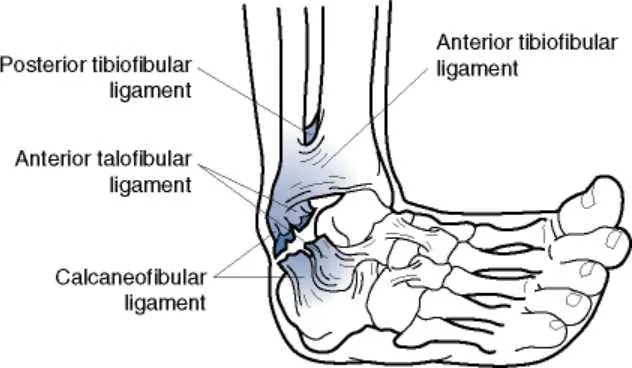
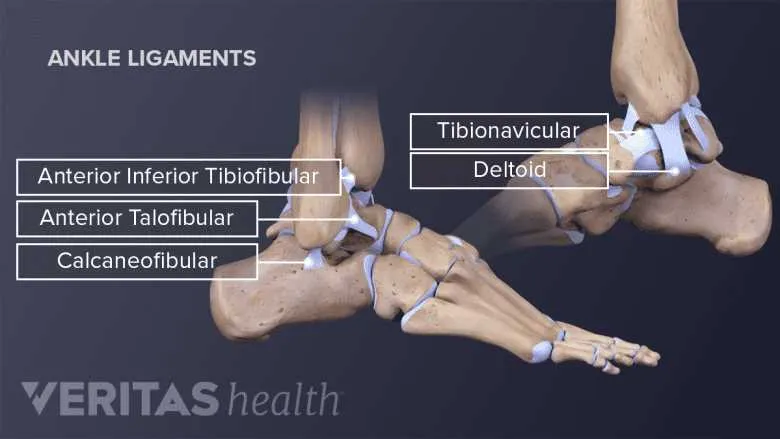
When a foot joint is injured, several muscles and ligaments are directly impacted, leading to pain, swelling, and limited mobility. These structures are critical for stabilizing the foot and enabling normal movement patterns. The following are the primary muscles and ligaments affected:
- Anterior Talofibular Ligament (ATFL) – This ligament is the most commonly damaged, especially in lateral injuries. It connects the fibula to the talus bone and provides stability during foot rotation.
- Calcaneofibular Ligament (CFL) – Positioned just below the ATFL, the CFL stabilizes the heel and prevents excessive rolling of the foot.
- Posterior Talofibular Ligament (PTFL) – Though less commonly injured, it plays a vital role in preventing backward movement of the talus, especially in severe cases.
- Peroneal Muscles – The peroneus longus and brevis muscles are crucial for foot eversion. These muscles can be strained or overstretched, contributing to discomfort and instability.
- Tibialis Anterior – A key muscle for dorsiflexion, its function can be compromised, resulting in difficulty lifting the foot.
- Flexor Hallucis Longus – This muscle helps in toe flexion, and its injury can hinder movements requiring strong push-off from the toes.
It is important to understand the role of these structures when managing recovery, as targeted rehabilitation can help restore function and strength to the affected areas.
Steps for Immediate Care and First Aid for a Sprained Ankle
Apply cold compression immediately using a gel ice pack or a bag of frozen vegetables wrapped in cloth. Limit exposure to 15–20 minutes every 2–3 hours during the first 48 hours to minimize swelling and tissue damage.
Elevate the affected limb above heart level using pillows, especially during rest or sleep, to reduce fluid accumulation and internal pressure.
Avoid weight-bearing activities. Use crutches or a walking boot to prevent further ligament strain and promote healing.
Secure the injured joint with an elastic bandage or compression wrap. Begin wrapping from the toes upward, applying even tension to support soft tissue without obstructing circulation.
Administer non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen to manage pain and inflammation. Follow dosage instructions strictly and consult a healthcare provider if symptoms persist beyond 72 hours.