When studying microorganisms, recognizing the points of intersection between these two groups is crucial. Despite being distinct in many ways, they share certain characteristics that can be important for understanding infections, treatments, and their role in ecosystems.
Cellular structure is one area where the differences are clear. One group consists of complex cells with a full structure, while the other lacks cellular machinery, relying instead on host cells for replication. However, both types can be pathogenic, affecting hosts in different ways, from mild illnesses to life-threatening conditions.
Another common trait is their ability to adapt rapidly to new environments. This shared adaptability makes studying their interactions with other organisms and the environment a vital part of medical research. Understanding these overlapping aspects can lead to better diagnostic methods and treatment strategies.
Comparison of Microorganisms: Key Differences and Overlaps
When studying microorganisms, it’s crucial to recognize the distinct characteristics that separate prokaryotic life forms from submicroscopic infectious agents. Prokaryotes are self-replicating cells, typically ranging from 0.5 to 5 micrometers, with a simple cellular structure, including a cell wall, plasma membrane, and circular DNA. They thrive in a wide range of environments and can reproduce independently through binary fission.
In contrast, infectious agents, which are not considered living organisms, require a host cell to reproduce. These entities are much smaller, with sizes ranging from 20 to 300 nanometers. They consist of either RNA or DNA encased in a protein coat, lacking any cellular structure such as a cell wall or internal machinery for metabolic processes.
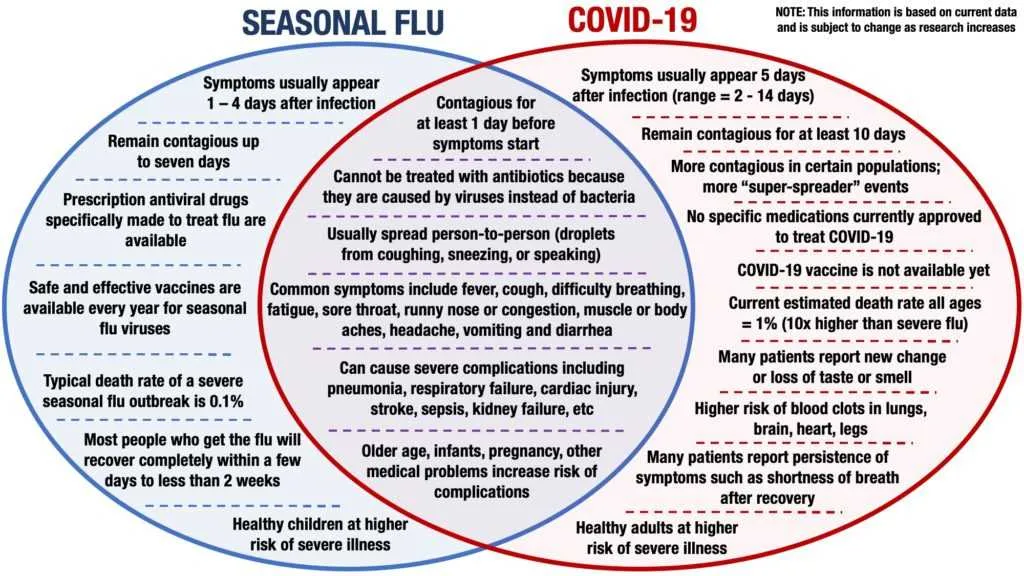
However, both types share similarities in their ability to evolve, adapt, and cause diseases in humans, animals, and plants. Both rely on genetic material to carry out their functions, though in vastly different ways. While the first can thrive on their own, the latter depends entirely on invading host cells to reproduce and propagate.
Despite these contrasts, both have been central to scientific research, particularly in the fields of medicine and biotechnology, as they contribute to human health, and are targets for treatments, vaccines, and research on antibiotic resistance.
Key Structural Differences
The main distinction between these two organisms lies in their structure. One is a single-cell entity with a complex internal system, including a cell membrane, cytoplasm, and genetic material (DNA or RNA). The other consists only of a protein coat and genetic material, which can either be RNA or DNA, but never both. The first type has ribosomes to synthesize proteins, while the second relies on a host cell’s machinery to replicate.
The presence of a cell wall distinguishes the first from the second, which lacks this feature. The first type may also have specialized appendages like flagella or pili for movement or adhesion, absent in the second type. The complexity of the first’s internal systems allows it to reproduce independently, unlike the second, which requires a host cell for replication.
How Microorganisms Interact with Host Cells
To prevent infections, it’s critical to understand the mechanisms through which pathogens invade host organisms. Pathogenic microorganisms use various methods to attach to and enter cells. Some exploit specific receptors on the host cell surface, while others may manipulate host cell processes to facilitate entry.
Once inside, these microbes hijack the host’s cellular machinery. Certain microorganisms release proteins that alter host cell functions, ensuring their survival and replication. In some cases, the host’s immune response can be triggered, resulting in inflammation and tissue damage as a side effect of the interaction.
To effectively block or minimize pathogenic invasion, targeting the adhesion mechanisms and preventing the entry of these harmful agents into the host cell is crucial. Additionally, understanding how these invaders manipulate host immune responses can inform vaccine development and therapeutic strategies.
Monitoring these interactions at the molecular level can help develop novel treatments aimed at disrupting pathogen-host cell dynamics, offering a more targeted approach to infection control.
Practical Applications: Identifying and Treating Infections
To effectively manage microbial infections, a clear understanding of the pathogen type is crucial for selecting the appropriate treatment approach.
- Rapid Diagnostic Testing: Immediate identification through PCR or antigen tests helps distinguish between microbial agents, guiding proper therapy.
- Targeted Antimicrobials: When dealing with bacterial infections, antibiotics like penicillin or tetracycline are commonly prescribed. For viral infections, antiviral agents such as oseltamivir or acyclovir are used.
- Symptom Management: Fever reducers (e.g., acetaminophen) and fluids can assist in relieving discomfort, but they should not replace pathogen-specific treatment.
Accurate distinction between these microorganisms can prevent misdiagnosis and avoid the use of inappropriate treatments, which can lead to resistance or prolonged illness.
Key Considerations for Treatment
- Duration of Illness: Chronic or persistent infections may require a different treatment regimen compared to acute cases.
- Severity of Infection: Mild infections can often be managed with over-the-counter medications, while severe cases may necessitate hospitalization or specialized care.
- Comorbidities: Existing health conditions like diabetes or immunosuppression influence treatment choices and patient management.
Understanding the distinctions between microbial pathogens is essential for healthcare providers to offer the most effective care and minimize complications.